EVERETT — At any given time, about 100 people are stuck in hospital beds at Providence Regional Medical Center Everett for months, or even years, longer than necessary.
Providence Everett exceeds patient capacity across all departments and has one of the busiest emergency departments in the state. It’s one of just two hospitals in the region that perform life-saving procedures for victims of Level 2 trauma, such as a heart attack or stroke.
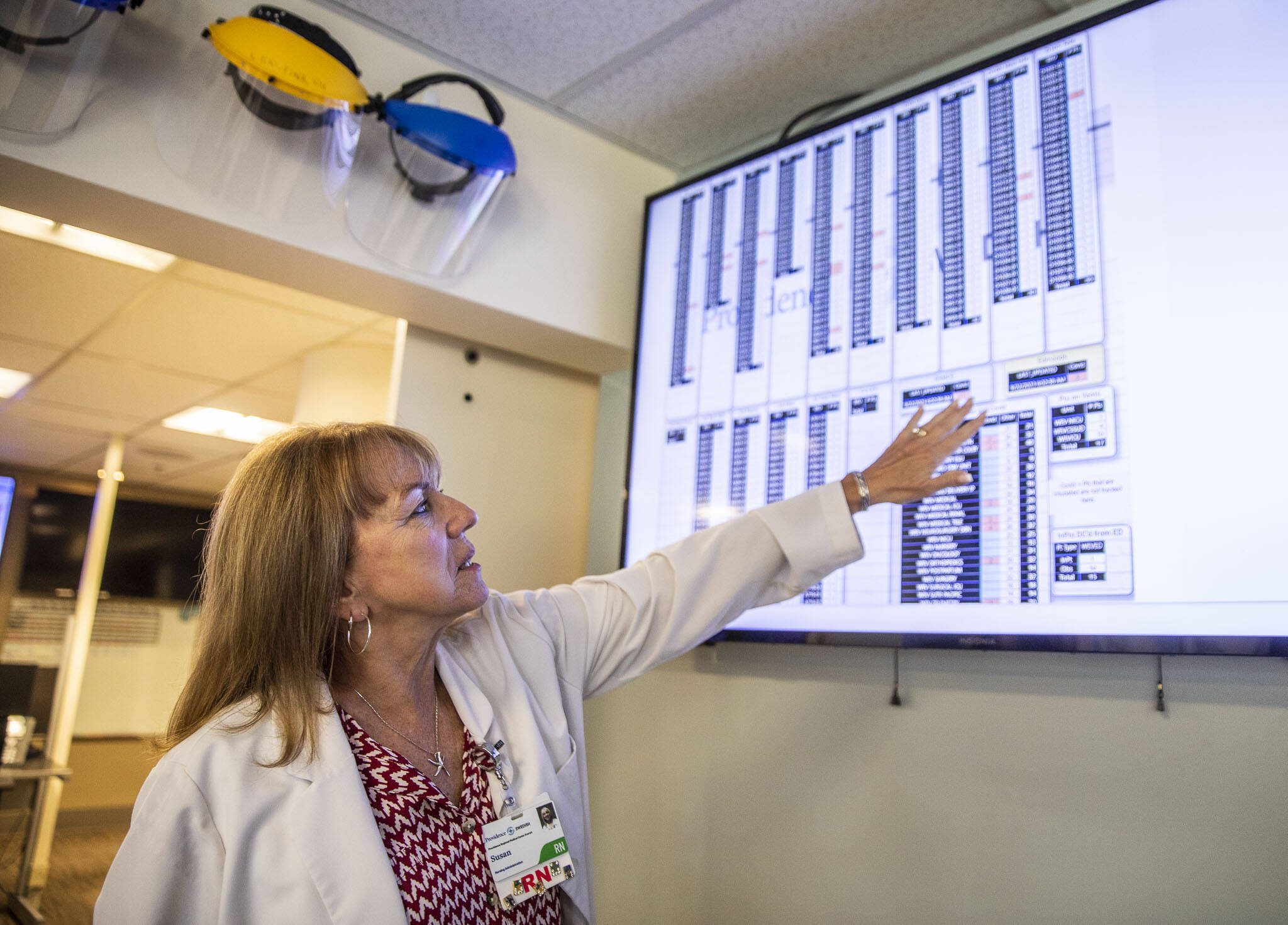
The hospital’s beds, 600 total across two campuses, are often full or unavailable because of a nurse staffing crisis. Some hospital staff spend their day in the control room, where large electronic boards keep track of patient check-ins and discharges, trying to decide which patients can go where like a game of Tetris.
Susan Williams, an administrative supervisor who has worked at Providence for 50 years, said the hospital has been over capacity for at least a decade — but it’s getting worse.
“It almost feels worse than before COVID,” she said. “We’ve had 19 discharges so far today. We need more like 70.”
Most hospital stays are a few hours, maybe a few days. Some patients, however, are medically stable but have long-term care needs the hospital must address before the patient can leave. This keeps them checked in for months or even years, leaving fewer beds for patients in acute distress.
This capacity crisis is statewide. Washington has fewer hospital beds per capita than any other state, and one to two of every 10 beds are occupied by patients who don’t need to be there, according to the Washington State Hospital Association.
It’s a predicament that can sink hospitals deeper into red ink, leave little room for sick patients and further strain an already overburdened hospital staff.
Medical limbo
Hospitals like Providence are seeing some of the worst budget deficits since early 2020 in part because of these longer stays, according to the state hospital association. A statewide survey published in March showed total hospital losses grew to $2.7 billion by the end of 2022.
There’s one glaring reason for this: Most insurers pay for hospital visits with fixed rates based on patient diagnosis, regardless of how long a patient stays. Once that money runs out, the hospital often foots the bill — up to $10,000 dollars a day.
A typical patient stay costs Providence $918 per day, on average, spokesperson Erika Hermanson said. State law requires Medicaid to pay hospitals a daily administrative rate, and cover services like dialysis or labs if the patient qualifies. If approved, the administrative payment covers less than half of daily costs per patient.
Providence reports showed costs outpaced revenue and its hospitals “continued to absorb the increased cost of caring for patients” in the first three months of 2023.
Providence Everett’s care management team coordinates next steps for patients so they can leave the hospital, a process called discharge planning. This can mean working with insurance to settle payment for a new walker, or finding available slots at assisted living, behavioral health and skilled nursing facilities.
Catherine Ambrose, senior director of care management for Providence Everett and Swedish Edmonds, said about one-third of patients at the Everett hospital need discharge planning.
“It’s one of those things you don’t know about until you need it, or a loved one needs it,” she said.
Jamie Park, the hospital’s chief medical officer, said current records show 76 people are caught in this medical limbo. The category is not easily defined, he added, and in reality there are about 100 patients stuck at the hospital on a regular basis.
Ambrose said she knew a patient who stayed at the Everett hospital for over two years.
“Hospitals are a safety net with resources,” she said. “They’re an option of last resort for people who have been failed by our society.”
Some patients face barriers that make discharge planning complicated. They may not have housing, insurance, citizenship documents or proper guardianship. If a patient can’t make decisions for themselves, state law prevents family or friends from signing off on a new care facility or approving Medicaid use on their behalf.
It takes about six weeks to appoint a legal guardian, and much longer if the patient doesn’t have anyone to take the role, Ambrose said. In that case, the hospital must go to court to appoint a certified professional guardian.
“What affects the least of us affects all of us,” Park said. “We need to come up with solutions.”
A Herald reporter asked to speak with patients in limbo at Providence Everett, but the hospital declined to provide names, citing its privacy policy.
‘It’s not a great place to live’
At least one-third of the patients who need discharge planning are waiting for transfer to long-term care, Ambrose said. Most hospital staff are trained to provide acute care, but don’t have the skill set or time to care for patients with long-term needs.
Patients in the hospital can miss out on opportunities offered at other facilities such as daily activities, community resources, extensive time outside or regular grooming, like haircuts.
“A hospital is a great place to get treatment for an illness or injury, but it’s not a great place to live,” said Ashlen Strong, vice president of government affairs at the state hospital association. “You can’t exercise, have social activities or get an education.”
Yet most other facilities are just as full as hospitals, facing severe financial strain and struggling to keep staff. Long-term care workers are among the lowest-paid in health care, according to LeadingAge Washington, a nonprofit advocating for senior care organizations.
“Long-term care has a staffing shortage right now,” said Alyssa Odegaard, vice president of public policy at the nonprofit. “We don’t have the ability to admit a lot of individuals from the hospital, especially ones who tend to have more complex needs.”
Odegaard said care facilities have to be picky. Patients with felony records or serious behavioral health disorders, for example, are less likely to be taken in.
“It’s really hard to discharge somebody from long-term care — another thing most providers hesitate to admit about why some of these individuals are stuck in the hospital,” Odegaard said.
Ambrose said when the pandemic hit, the state provided incentives for care facilities to accept patients. The need is still there, she said, but the money has dried up.
The state’s priority is ensuring patients are ready for discharge and can last in a long-term care setting, said Jacqueine Cobbs, deputy director for the state Department of Social and Health Services’ Home and Community Services division.
“They need to be medically and psychiatrically stable, able to receive help and function at a lesser-level of care,” she said. “There is a need for communication and collaboration, as opposed to just incentivizing providers. If they’re not able to meet an individual’s needs, that person will be right back into a hospital. We want them to not just transition from a setting, but remain stable and safe in the community.”
‘This is a crisis for us’
Providence leadership said they’ve partnered with skilled nursing facility Bethany of the Northwest to staff 60 beds on the Pacific campus with long-term care workers — but they need more help.
“Our government affairs team went to the state and told them, ‘This is a crisis for us,’” Ambrose said.
State Sen. June Robinson, D-Everett, who has worked for years to help address discharge challenges at Providence, said there’s no simple solution.
“We don’t have facilities that are equipped for people with complex needs,” said Robinson, who serves as vice chair of the state Senate’s Health and Long Term Care Committee. “Ultimately, the people who are in that situation are suffering.”
Last year, the state invested over $91 million to help hospitals discharge patients. The money has gone to mass certification sites for nursing assistants, care management support and incentives for long-term care providers that have resulted in over 100 more discharges per month, according to the state. State money has also funded stays for undocumented patients and certified professional guardian contracts.
In this year’s legislative session, state lawmakers agreed to increase Medicaid reimbursement rates to long-term care facilities, behavioral health providers and hospitals. Using a federal dollar-matching program similar to other states, lawmakers predict an additional $1 billion in hospital funding starting in 2024.
State lawmakers also agreed to allocate over $500 million to address discharge delays, including a new “discharge task force” of elected officials and medical experts. The task force will oversee a two-year pilot program — based on a patient discharge model created by Harborview Medical Center in Seattle — at Providence Everett and four other hospitals.
Ambrose, who is helping lead the program at Providence, said the pilot is in early development.
“We’re excited to be a part of it,” she said. “There’s a lot of eagerness to look at what we can do.”
Zosia Stanley, vice president of the Washington State Hospital Association, represents the association on the task force. She said the goal of the pilot program is to collect data and determine the need for state-funded care services that hospitals and long-term facilities can’t always offer.
“With these wraparound services,” Stanley said, “patients could get back into the community.”
Sydney Jackson: 425-339-3430; sydney.jackson@heraldnet.com; Twitter: @_sydneyajackson.
Talk to us
> Give us your news tips.
> Send us a letter to the editor.
> More Herald contact information.